NEET MDS Lessons
Orthodontics
Nail Biting Habits
Nail biting, also known as onychophagia, is one of the most common habits observed in children and can persist into adulthood. It is often associated with internal tension, anxiety, or stress. Understanding the etiology, clinical features, and management strategies for nail biting is essential for addressing this habit effectively.
Etiology
-
Emotional Problems:
- Persistent nail biting may indicate underlying emotional issues, such as anxiety, stress, or tension. It can serve as a coping mechanism for dealing with these feelings.
-
Psychosomatic Factors:
- Nail biting can be a psychosomatic response to stress or emotional discomfort, manifesting physically as a way to relieve tension.
-
Successor of Thumb Sucking:
- For some children, nail biting may develop as a successor to thumb sucking, particularly as they transition from one habit to another.
Clinical Features
-
Dental Effects:
- Crowding: Nail biting can contribute to dental crowding, particularly if the habit leads to changes in the position of the teeth.
- Rotation: Teeth may become rotated or misaligned due to the pressure exerted during nail biting.
- Alteration of Incisal Edges: The incisal edges of the anterior teeth may become worn down or altered due to repeated contact with the nails.
-
Soft Tissue Changes:
- Inflammation of Nail Bed: Chronic nail biting can lead to inflammation and infection of the nail bed, resulting in redness, swelling, and discomfort.
Management
-
Awareness:
- The first step in management is to make the patient aware of their nail biting habit. Understanding the habit's impact on their health and appearance can motivate change.
-
Addressing Emotional Factors:
- It is important to identify and treat any underlying emotional issues contributing to the habit. This may involve counseling or therapy to help the individual cope with stress and anxiety.
-
Encouraging Outdoor Activities:
- Engaging in outdoor activities and physical exercise can help reduce tension and provide a positive outlet for stress, potentially decreasing the urge to bite nails.
-
Behavioral Modifications:
- Nail Polish: Applying a bitter-tasting nail polish can deter nail biting by making the nails unpalatable.
- Light Cotton Mittens: Wearing mittens or gloves can serve as a physical reminder to avoid nail biting and can help break the habit.
-
Positive Reinforcement:
- Encouraging and rewarding the individual for not biting their nails can help reinforce positive behavior and motivate them to stop.
Theories of Tooth Movement
-
Pressure-Tension Theory:
- Concept: This theory posits that tooth movement occurs in response to the application of forces that create areas of pressure and tension in the periodontal ligament (PDL).
- Mechanism: When a force is applied to a tooth, the side of the tooth experiencing pressure (compression) leads to bone resorption, while the opposite side experiences tension, promoting bone deposition. This differential response allows the tooth to move in the direction of the applied force.
- Clinical Relevance: This theory underlies the rationale for using light, continuous forces in orthodontic treatment to facilitate tooth movement without causing damage to the periodontal tissues.
-
Biological Response Theory:
- Concept: This theory emphasizes the biological response of the periodontal ligament and surrounding tissues to mechanical forces.
- Mechanism: The application of force leads to a cascade of biological events, including the release of signaling molecules that stimulate osteoclasts (bone resorption) and osteoblasts (bone formation). This process is influenced by the magnitude, duration, and direction of the applied forces.
- Clinical Relevance: Understanding the biological response helps orthodontists optimize force application to achieve desired tooth movement while minimizing adverse effects.
-
Cortical Bone Theory:
- Concept: This theory focuses on the role of cortical bone in tooth movement.
- Mechanism: It suggests that the movement of teeth is influenced by the remodeling of cortical bone, which is denser and less responsive than the trabecular bone. The movement of teeth through the cortical bone requires greater forces and longer durations of application.
- Clinical Relevance: This theory highlights the importance of considering the surrounding bone structure when planning orthodontic treatment, especially in cases requiring significant tooth movement.
Primate spaces, also known as simian spaces or anthropoid spaces, are specific gaps that occur in the dental arch of children during the mixed dentition phase. These spaces are significant in the development of the dental arch and play a role in accommodating the eruption of permanent teeth.
Characteristics of Primate Spaces
-
Location:
- Maxillary Arch: Primate spaces are found mesial to the primary maxillary canines.
- Mandibular Arch: They are located distal to the primary mandibular canines.
-
Significance:
- Primate spaces are natural spaces that exist between primary teeth.
They are important for:
- Eruption of Permanent Teeth: These spaces help accommodate the larger size of the permanent teeth that will erupt later.
- Alignment: They assist in maintaining proper alignment of the dental arch as the primary teeth are replaced by permanent teeth.
- Primate spaces are natural spaces that exist between primary teeth.
They are important for:
-
Naming:
- The term "primate spaces" is derived from the observation that similar spaces are found in the dentition of non-human primates. The presence of these spaces in both humans and primates suggests a common evolutionary trait related to dental development.
Clinical Relevance
- Monitoring Development: The presence and size of primate spaces can be monitored by dental professionals to assess normal dental development in children.
- Orthodontic Considerations: Understanding the role of primate spaces is important in orthodontics, as they can influence the timing and sequence of tooth eruption and the overall alignment of the dental arch.
- Space Maintenance: If primary teeth are lost prematurely, the absence of primate spaces can lead to crowding or misalignment of the permanent teeth, necessitating the use of space maintainers or other orthodontic interventions.
Quad helix appliance is an orthodontic device used to expand the upper arch of teeth. It is typically cemented to the molars and features a U-shaped stainless steel wire with active helix springs, helping to correct issues like crossbites, narrow jaws, and crowded teeth. ### Components of the Quad Helix Appliance
-
Helix Springs:
- The appliance contains two or four active helix springs that exert gentle pressure to widen the dental arch.
-
Bands:
- It is attached to the molars using bands, which provide a stable anchor for the appliance.
-
Wire Framework:
- Made from 38 mil stainless steel wire, the framework allows for customization and adjustment by the orthodontist.
Functions of the Quad Helix Appliance
-
Arch Expansion:
- The primary function is to gradually widen the upper arch, creating more space for crowded teeth.
-
Correction of Crossbites:
- It helps in correcting posterior crossbites, where the lower teeth are positioned outside the upper teeth.
-
Molar Stabilization:
- The appliance stabilizes the molars in their correct position during treatment.
Indications for Use
-
Narrow Upper Jaw:
- Ideal for patients with a constricted upper arch.
-
Crowded Teeth:
- Used when there is insufficient space for teeth to align properly.
-
Class II and Class III Cases:
- Effective in treating specific malocclusions that require arch expansion.
Advantages of the Quad Helix Appliance
-
Non-Invasive:
- It is a non-surgical option for expanding the dental arch.
-
Fixed Design:
- As a fixed appliance, it does not rely on patient compliance for activation.
-
Customizable:
- The design allows for adjustments to meet individual patient needs.
Limitations of the Quad Helix Appliance
-
Initial Discomfort:
- Patients may experience mild discomfort or pressure during the first few weeks of use.
-
Oral Hygiene Challenges:
- Maintaining oral hygiene can be more difficult, requiring diligent cleaning around the appliance.
-
Adjustment Period:
- It may take time for patients to adapt to speaking and swallowing with the appliance in place.
Growth is the increase in size It may also be defined as the normal change in the amount of living substance. eg. Growth is the quantitative aspect and measures in units of increase per unit of time.
Development
It is the progress towards maturity (Todd). Development may be defined as natural sequential series of events between fertilization of ovum and adult stage.
Maturation
It is a period of stabilization brought by growth and development.
CEPHALOCAUDAL GRADIENT OF GROWTH
This simply means that there is an axis of increased growth extending from the head towards feet. At about 3rd month of intrauterine life the head takes up about 50% of total body length. At this stage cranium is larger relative to face. In contrast the limbs are underdeveloped.
By the time of birth limbs and trunk have grown faster than head and the entire proportion of the body to the head has increased. These processes of growth continue till adult.
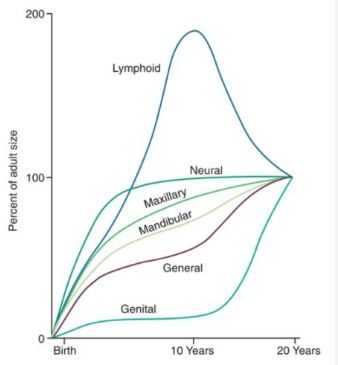
SCAMMON’S CURVE
In normal growth pattern all the tissue system of the body do not growth at the same rate. Scammon’s curve for growth shows 4 major tissue system of the body;
• Neural
• Lymphoid
• General: Bone, viscera, muscle.
• Genital
The graph indicates the growth of the neural tissue is complete by 6-7 year of age. General body tissue show an “S” shaped curve with showing of rate during childhood and acceleration at puberty. Lymphoid tissues proliferate to its maximum in late childhood and undergo involution. At the same time growth of the genital tissue accelerate rapidly.
Springs in Orthodontics
Springs are essential components of removable orthodontic appliances, playing a crucial role in facilitating tooth movement. Understanding the mechanics of springs, their classifications, and their applications is vital for effective orthodontic treatment.
- Springs are active components of removable orthodontic appliances that deliver forces to teeth and/or skeletal structures, inducing changes in their positions.
- Mechanics of Tooth Movement: To achieve effective tooth movement, it is essential to apply light and continuous forces. Heavy forces can lead to damage to the periodontium, root resorption, and other complications.
Components of a Removable Appliance
A removable orthodontic appliance typically consists of three main components:
- Baseplate: The foundation that holds the appliance together and provides stability.
- Active Components: These include springs, clasps, and other elements that exert forces on the teeth.
- Retention Components: These ensure that the appliance remains in place during treatment.
Springs as Active Components
Springs are integral to the active components of removable appliances. They are designed to exert specific forces on the teeth to achieve desired movements.
Components of a Spring
- Wire Material: Springs are typically made from stainless steel or other resilient materials that can withstand repeated deformation.
- Shape and Design: The design of the spring influences its force delivery and stability.
Classification of Springs
Springs can be classified based on various criteria:
1. Based on the Presence or Absence of Helix
- Simple Springs: These springs do not have a helix and are typically used for straightforward tooth movements.
- Compound Springs: These springs incorporate a helix, allowing for more complex movements and force applications.
2. Based on the Presence of Loop or Helix
- Helical Springs: These springs feature a helical design, which provides a continuous force over a range of motion.
- Looped Springs: These springs have a looped design, which can be used for specific tooth movements and adjustments.
3. Based on the Nature of Stability
- Self-Supported Springs: Made from thicker gauge wire, these springs can support themselves and maintain their shape during use.
- Supported Springs: Constructed from thinner gauge wire, these springs lack adequate stability and are often encased in a metallic tube to provide additional support.
Applications of Springs in Orthodontics
- Space Maintenance: Springs can be used to maintain space in the dental arch during the eruption of permanent teeth.
- Tooth Movement: Springs are employed to move teeth into desired positions, such as correcting crowding or aligning teeth.
- Retention: Springs can also be used in retainers to maintain the position of teeth after orthodontic treatment.
Headgear is an extraoral orthodontic appliance used to correct dental and skeletal discrepancies, particularly in growing patients. It is designed to apply forces to the teeth and jaws to achieve specific orthodontic goals, such as correcting overbites, underbites, and crossbites, as well as guiding the growth of the maxilla (upper jaw) and mandible (lower jaw). Below is an overview of headgear, its types, mechanisms of action, indications, advantages, and limitations.
Types of Headgear
-
Class II Headgear:
- Description: This type is used primarily to correct Class II malocclusions, where the upper teeth are positioned too far forward relative to the lower teeth.
- Mechanism: It typically consists of a facebow that attaches to the maxillary molars and is anchored to a neck strap or a forehead strap. The appliance applies a backward force to the maxilla, helping to reposition it and/or retract the upper incisors.
-
Class III Headgear:
- Description: Used to correct Class III malocclusions, where the lower teeth are positioned too far forward relative to the upper teeth.
- Mechanism: This type of headgear may use a reverse-pull face mask that applies forward and upward forces to the maxilla, encouraging its growth and improving the relationship between the upper and lower jaws.
-
Cervical Headgear:
- Description: This type is used to control the growth of the maxilla and is often used in conjunction with other orthodontic appliances.
- Mechanism: It consists of a neck strap that connects to a facebow, applying forces to the maxilla to restrict its forward growth while allowing the mandible to grow.
-
High-Pull Headgear:
- Description: This type is used to control the vertical growth of the maxilla and is often used in cases with deep overbites.
- Mechanism: It features a head strap that connects to the facebow and applies upward and backward forces to the maxilla.
Mechanism of Action
- Force Application: Headgear applies extraoral forces to
the teeth and jaws, influencing their position and growth. The forces can be
directed to:
- Restrict maxillary growth: In Class II cases, headgear can help prevent the maxilla from growing too far forward.
- Promote maxillary growth: In Class III cases, headgear can encourage forward growth of the maxilla.
- Reposition teeth: By applying forces to the molars, headgear can help align the dental arches and improve occlusion.
Indications for Use
- Class II Malocclusion: To correct overbites and improve the relationship between the upper and lower teeth.
- Class III Malocclusion: To promote the growth of the maxilla and improve the occlusal relationship.
- Crowding: To create space for teeth by retracting the upper incisors.
- Facial Aesthetics: To improve the overall facial profile and aesthetics by modifying jaw relationships.
Advantages of Headgear
- Non-Surgical Option: Provides a way to correct skeletal discrepancies without the need for surgical intervention.
- Effective for Growth Modification: Particularly useful in growing patients, as it can influence the growth of the jaws.
- Improves Aesthetics: Can enhance facial aesthetics by correcting jaw relationships and improving the smile.
Limitations of Headgear
- Patient Compliance: The effectiveness of headgear relies heavily on patient compliance. Patients must wear the appliance as prescribed (often 12-14 hours a day) for optimal results.
- Discomfort: Patients may experience discomfort or soreness when first using headgear, which can affect compliance.
- Adjustment Period: It may take time for patients to adjust to wearing headgear, and they may need guidance on how to use it properly.
- Limited Effectiveness in Adults: While headgear is effective in growing patients, its effectiveness may be limited in adults due to the maturity of the skeletal structures.
